Category: Resource
-
Relentless Love: What a Foster Cat Mom Teaches Us About Attachment and Trauma
Recently, I watched a short video of a foster mother cat gently caring for a kitten who had clearly endured trauma. The kitten flinched at every movement, tucked itself into corners, and froze at any attempt at touch. But the mother cat didn’t retreat. She moved slowly, calmly—relentlessly. With every lick, every soft purr, every patient pause, she sent the same message: You are safe now. I won’t hurt you. I’m not going anywhere.
As I watched, I realized: this is exactly what it looks like to build attachment with a child who has experienced complex developmental trauma.
In Ecosystemic Structural Family Therapy (ESFT), we talk about the importance of reestablishing safety and connection as the foundation of all therapeutic work. For children who have learned through experience that adults are unpredictable, unavailable, or unsafe, attachment isn’t automatic—it must be earned through consistency, patience, and deep emotional attunement.
The caregiver’s role is to embody safety. Not to demand closeness, but to offer connection without pressure, and to remain emotionally available even in the face of rejection or withdrawal. Just like the foster mother cat, the caregiver must be willing to show up again and again, saying with their actions:
💬 I see you.
💬 Your fear makes sense. I would be afraid too.
💬 I’ll stay until you trust.Attachment doesn’t come from grand gestures—it comes from the quiet, repeated moments of co-regulation: sharing calm, honoring the child’s emotional state, and staying present without needing immediate results.
In a trauma-informed, strength-based model like ESFT, we understand that healing happens through relationship, not in spite of it. And while the journey is slow, the impact is profound.
That tiny kitten eventually crept toward the mother cat and tucked itself under her warmth. It didn’t happen all at once—but it happened. The same is possible for the children we serve.
Traumatized children don’t need perfect caregivers. They need relentless ones. Ones who stay. Ones who wait. Ones who whisper safety through every calm breath and patient act of love.
Because healing begins where fear once lived—and trust is the bridge we build one steady step at a time.
-
Wear Sunscreen—and Practice ESFT: Life Advice Meets Systemic Family Therapy
If you’ve ever heard the iconic spoken-word song “Everybody’s Free (To Wear Sunscreen),” you know it’s packed with practical, poetic, and unexpectedly emotional advice. Originally a column by Mary Schmich and popularized by Baz Luhrmann, the song reads like a love letter to life’s complexity—with one recurring reminder: wear sunscreen.
But if you listen closely, the heart of the song is about more than sun protection—it’s about perspective. It’s about embracing uncertainty, holding paradoxes, and trusting that life is rarely linear. And if there’s any therapeutic model that echoes that spirit, it’s Ecosystemic Structural Family Therapy (ESFT) – making the complex simple by seeing the challenge as relational not behavioral.
“Don’t waste your time on jealousy. Sometimes you’re ahead, sometimes you’re behind. The race is long—and in the end, it’s only with yourself.”
In ESFT, we often help families move away from competitive, comparison-based narratives and toward shared emotional connection. Healing happens when we shift from proving or winning to joining and reframing. Families don’t need perfect answers—they need safe spaces to be seen, to struggle, and to grow.
“Do one thing every day that scares you.”
In the family therapy room, vulnerability is that one thing. Asking a caregiver to hold limits with love, encouraging a teen to share hurt instead of anger, or guiding a therapist-in-training to sit in discomfort—these are ESFT moments. Progress isn’t comfortable; it’s courageous action inside safe structure.
“Be kind to your knees. You’ll miss them when they’re gone.”
We help families appreciate the everyday, not just the crisis. ESFT is a model rooted in social ecology, reminding us that growth doesn’t happen in isolation—it happens in schools, homes, neighborhoods, and quiet moments. The small, unseen strengths families already possess often become their greatest tools for change.
The Therapist’s Sunscreen? Structure.
Just as sunscreen protects us from invisible harm, structure protects families from the chaos of unchecked patterns. The ESFT therapist holds that structure so families can safely explore their agency. We aren’t rescuers—we’re guides walking families toward their own power.
In a way, wear sunscreen is exactly what we ask families to do: protect what matters, risk connection, trust the process—and be gentle with yourselves.
-
Burnout and Feedback: Holding Your Work Without Losing Yourself
Therapists are often told to stay reflective, take feedback in stride, and manage their energy. But when you’re experiencing emotional burnout, even minor criticism from a client can feel overwhelming.
Burnout isn’t a sign that you’re doing something wrong—it’s often a sign that you’ve been giving without enough replenishment. And when that’s paired with negative client feedback, it can create self-doubt and isolation.
Systemic family therapists are trained to hold complexity, but we often forget that we are also part of the system. We are influenced by the emotional load we carry, and by the stories we witness. If we don’t build structures of care around ourselves, we start to lose the clarity and compassion that make this work meaningful.
Negative feedback doesn’t have to be internalized—it can be contextualized. Ask: Is this about the therapeutic relationship? A reaction to change? A reflection of broader stress in the system?
More importantly, how are you tending to yourself? Supervision, peer support, and even a quiet walk after a tough session are not luxuries—they’re necessities. Therapists can’t pour from an empty cup. We need to refill regularly, and permission ourselves to rest without guilt.
-
When Time is Tight: Engaging the Whole Family in Brief Moments
Engaging every member of a family in therapy is no small feat. In many sessions, one or two voices dominate while others fade into the background. Add in tight session times, and it’s tempting to focus on immediate issues rather than broad engagement.
But presence matters more than perfection. The goal isn’t to fix every dynamic in one session—it’s to build small, intentional moments of connection across time. Each session is a stepping stone toward larger transformation.
Start by redefining success. Engagement doesn’t always mean equal talk time. It might mean one small contribution from a typically silent member. It might look like a validating nod or a moment of shared laughter. These moments matter.
Time constraints force us to be strategic:
- Use change enactments to invite all members to speak without pressure.
- Set clear, attainable goals for each session.
- Circle back to quieter members and validate their presence, even if they say little.
Remember, engagement is not a single moment—it’s a relationship built over time. The more consistent and inclusive the therapist’s approach, the more likely family members are to show up not just physically, but emotionally.
-
Turning Resistance into Communication Opportunities

Resistance from clients is one of the most common and frustrating challenges therapists face. Whether it’s missed appointments, shutdowns in session, or flat-out refusal to engage, resistance can feel like a personal failure or a sign that therapy isn’t working. But what if resistance is actually a form of communication?
In systemic family therapy, we reframe resistance not as opposition, but as protection. Often, clients resist because they feel vulnerable, uncertain, or unheard. In fact, that resistance may be signaling something crucial: a desire for improved family communication but a fear of the discomfort or change that might come with it.
By approaching resistance with curiosity rather than control, we open a door to deeper engagement. Instead of asking “Why won’t they cooperate?” we ask, “What are they trying to protect? What do they need to feel safe enough to participate?” This shift reframes resistance as a relational signal—not a defect.
Therapists can leverage moments of resistance by validating the client’s concerns and aligning with their underlying needs. Resistance often melts when a client feels truly seen and heard—especially when they’re struggling to find their voice in a complicated family system.
Improved family communication is not a byproduct of therapy—it’s a central goal. When resistance arises, it’s a cue that the path to better communication is available—but not yet accessible. Our role is to guide the family toward it by leaning into discomfort, modeling vulnerability, and keeping the relational frame intact.
-
💡 Why a Strength-Based, Relational Approach Matters💡
When families are navigating behavioral challenges — whether it’s a child acting out, conflict between siblings, or ongoing tension between caregivers — the natural impulse is to turn to the therapist as the “expert” to fix the problem. In that moment, families often believe that they have little to offer, that the solution must come from outside of them, and that their relationships and history have little to do with the issue at hand.
But as systemic family therapists, we know that this approach is incomplete. In fact, it can be harmful. When families start to believe they are powerless in the face of problems, they become passive observers rather than active participants in their own growth. And when therapists reinforce this dynamic — intentionally or not — we rob families of their agency and diminish the power of the relational system.
A strength-based, relational approach turns this on its head.
Rather than focusing solely on what’s broken, we look for what’s working — the small moments of connection, care, resilience, and effort that already exist within the family system. We ask ourselves:
- Where are the strengths hiding in plain sight?
- How can we build on those to address behavioral challenges together?
- What has this family survived, overcome, or adapted to before?
This perspective allows us to solve problems relationally, not just behaviorally. A child’s acting-out behavior isn’t addressed in isolation but understood within the context of relationships, stressors, patterns, and roles in the family. We see behavior as communication, shaped by the family’s environment, expectations, and connection.
When families experience this shift, everything changes. They stop waiting for the expert to deliver answers and begin participating in creating solutions. They regain a sense of capability and confidence, recognizing that their relationships are not only part of the problem — but the foundation of the solution.
At PCFTTC, we believe that every family holds the raw material for their own healing. Our role is to uncover, name, and strengthen those existing resources while guiding families toward healthier, more connected ways of being together.
Strength-based, relational work isn’t about being soft — it’s about being strategic, respectful, and effective. It’s how we create change that lasts.
-
CHECK OUT THIS ARTICLE FROM McCrystal Group: Adaptable, But Anchored: The Hidden Strength of Character in Leadership
Fast can be fragile. Adaptability without character can break when it matters most.
Nearly a decade ago, Team of Teams changed how we think about building organizations. It showed us that in complex, high-velocity environments, speed and adaptability come not from control but from trust, shared consciousness, common purpose, and empowered execution.
But, in a world of rapid technological change and moral booby traps around every corner, adaptability alone isn’t enough. Because what holds systems together under pressure isn’t just structure. It’s character.
The hidden variable in high-performing organizations isn’t just how you lead. It’s who you are while leading.That’s where On Character enters, the latest book from Stan McChrystal, examining the shifting focus from systems to the individual. Exceptional leaders don’t just drive results; they embody values like humility, integrity, and selflessness. These aren’t soft skills. They are the foundation of trust, loyalty, and long-term impact.
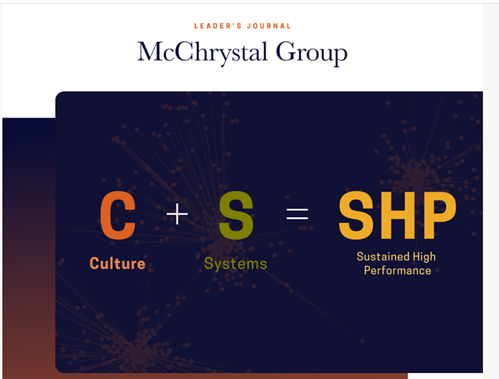
Together, Team of Teams and On Character offer a simple but profound truth:
You can build a highly adaptive organization, but it will only be as strong as the character of its members. Speed is necessary. Adaptability is required. But trust and character are what endure.
Leaders must question their convictions and consider how deep their values truly go. Ask yourself:
- Am I exhibiting the behaviors I expect of my people?
- Do my decisions reflect conviction or convenience?
- Would my team describe me as someone worth following, especially when it’s hard?
As you reflect on your own contribution to the “culture + system = sustained high-performance” equation, we invite you to explore our resources from the Team of Teams 10th Anniversary collection, designed to help leaders build adaptable systems and enduring character.
Related Insights:
- Leadership Behaviors Needed in a Complex World
- Lead Like a Gardener
- Team of Teams® Executive Summary Guide
- The 4 Secrets High-Performance Organizations Know About Teams
Copyright © 2025 McChrystal Group, All rights reserved.
-
The Power of Collective Support: What The Turnaround Teaches Us About Social Ecology and Strength-Based Practice
Netflix Link: https://www.netflix.com/us/title/81945091?s=i&trkid=258593161&vlang=en
In The Turnaround, a Netflix short documentary, we witness a rare and powerful moment in sports: a city choosing compassion over criticism. When Philadelphia Phillies shortstop Trea Turner struggled during the 2023 MLB season, the typical response might have been boos and frustration. But what happened instead was extraordinary—fan Jon McCann called for a standing ovation. The city responded. The crowd stood, cheered, and poured belief into a player at one of his lowest moments. What followed was a surge in Turner’s performance, and a deep emotional shift in how fans and athletes connected.
At PCFTTC, we see this moment as a real-world example of social ecology in action. Just like in therapy, healing and growth don’t happen in isolation. People are shaped by their environments—families, communities, systems of support. When one part of the system chooses empathy and encouragement over shame or blame, it reverberates.
Turner’s story reminds us why being strength-based and context-sensitive matters. His performance issues weren’t just about mechanics—they were about mindset, pressure, and the invisible weight of expectations. Instead of pathologizing the “problem” (Turner’s slump), the community looked at the context and chose to support rather than punish. In doing so, they acted as a trauma-informed system—offering safety, connection, and belief.
This is precisely the lens we use in Ecosystemic Structural Family Therapy (ESFT). When working with families, we don’t just treat behaviors—we look at the context that sustains them. We seek to understand before we intervene. We ask: what would happen if this family were met with belief instead of blame?
The Turnaround teaches us that systemic change begins with one choice: to hold dignity and possibility in the face of struggle. As therapists, supervisors, and healers, we can ask ourselves: how do we create our own “standing ovation” moments for the families we serve? How do we choose hope, every time?
Let this story inspire us to keep building systems of care that are trauma-informed, context-sensitive, and full of the kind of strength-based belief that can change lives.
